Freed from the clutches of snake oil medicine, Hyperbaric Oxygen Therapy (HBOT) is a drug-free, very safe, and calming modality that is also maybe one of the most innovative and adaptable healing and anti-aging therapies available today. However, it’s unlikely that you’ve heard of it. If you have, it was most likely for the therapy of diabetic foot ulcers, carbon monoxide poisoning, decompression sickness, or potentially necrotizing fasciitis. There is so much more that HBOT can accomplish, even while it is incredibly successful in treating all of these conditions
Evolution of Hyperbaric Medicine
A British clergyman Henshaw constructed an airtight chamber that was connected to an organ below in the 17th century. One might configure the organ below to either suction air out of the chamber or pump more air into it, compressing more air into a set area. An atmosphere that was pumped with air was referred to as hyperbaric. In contrast, a hypobaric environment is a chamber that has had its air forced out of it. Throughout the 18th and 19th centuries, it was believed that hyperbaric air was best used to cure acute illnesses while hypobaric air was best used to treat chronic illnesses like TB.
The therapy of decompression disease marked the beginning of contemporary hyperbaric medicine; this horrible illness still kills, paralyzes, or badly injures its victims. The number of persons afflicted by “the bends,” as it was once known, was astounding following the surge in suspension bridge construction from the middle to the end of the 19th century. Bridge workers were submerged in caissons, pressurized hyperbaric chambers located well below the water’s surface. When the workers sealed within the caissons and drilled down into the riverbed bottom to anchor the bridge pile-ons, the caissons were pressurized to keep water out. The “bends” would have been disastrous if these workers had been brought back up to the surface too soon via elevator shafts.
Crucially, though, was the discovery that these problems of workers disappeared once they went into the caissons once more. This happened in the late 19th century when the Brooklyn Bridge was being built. Some or all of the users’ problems were alleviated when they “toughed it out” and returned to the caisson the next day, regardless of how serious their injuries were.
The reason was straightforward and was also found by the end of the 19th century: at sea level, the air contained around 78% nitrogen and 21% oxygen. The water above the caisson workers put pressure on their breathing air while they were underwater. Henry’s Law states that despite the same gas ratios, there was a significant rise in the quantity of dissolved nitrogen and oxygen in the blood. Henry’s law—states that gas will transition more into a liquid form the greater pressure it is subjected to—is significant to hyperbaric medicine and deserves clarification. It turns out that the human body’s liquid state is found in blood plasma.
The issue with “the bends” stemmed from an overabundance of depressurization, which led to the large-scale bubble of nitrogen returning to gaseous form from blood circulation, potentially overwhelming circulatory flow. Micro and macrovascular ischemia was brought on by nitrogen gas, which essentially stopped blood flow to the tissues. The goal of therapy was to return those gas bubbles to a liquid state as quickly as possible by bringing the air pressure back to what it was before the deepsea divers and caisson worker surfaced.
This was precisely what a hyperbaric chamber could do, and before long, chambers were installed at building sites for bridges and subsequently at diving sites across the globe. Users with serious injuries, seizures, and paralysis might leave the chamber a few hours later with no symptoms. Although the outcomes were nothing short of extraordinary, they weren’t a miracle. The nitrogen bubbles were redissolved and blood flow was resumed using hyperbaric chambers.
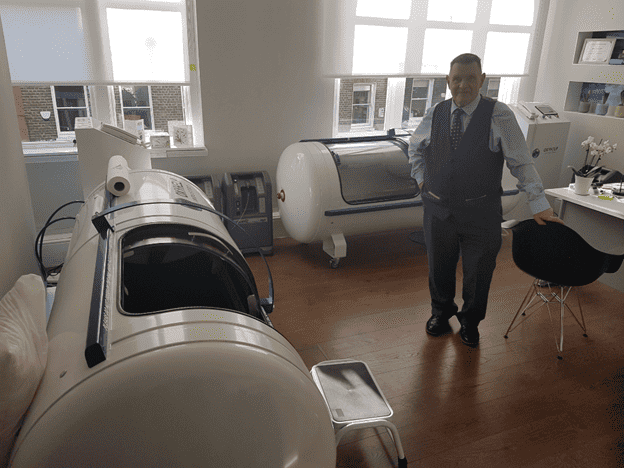
Inside the Hyperbaric Chamber
HBOT chambers come in three types: soft-bag chambers, hard-shelled monoplace chambers that handle a single user at a time, and hard-shelled multiplace chambers that treat many users simultaneously. The way that multiplace and monoplace chambers function is by raising the air pressure as the user inhales 95% oxygen. We now know that doing so can result in a markedly higher amount of oxygen dissolved into the blood circulation because of Henry’s Law. However, since 96% of the hemoglobin sites on red blood cells (RBCs) are saturated as they pass through lung capillaries in a healthy individual, this effect is not noticed at the level of RBCs.
Rather, oxygen is forced to levels in the blood plasma that can surpass 12 times that of sea level, or more than 1200%. At the tissue level, normal blood oxygen levels vary from 45 to 55 mmHg. When receiving HBOT, arterial O2 tension usually rises to 2000 mmHg or more, with body tissues occurring at values between 200 and 400 mmHg. It should be noted that, in general, the air compression in soft-bag chambers is not as deep as that in hard-shelled chambers.
Therapeutic Effects of HBOT
The supraphysiologic plasma oxygen concentration underlies the therapeutic impact of HBOT regardless of the chamber. An initial reversal of hypoxia, a reduction in inflammation, the optimization of all phases of wound healing, the revitalization of mitochondria, and the prevention of infection are the five particular ways in which this sets off a series of changes that might impact the body.
Applications of HBOT
Ischemic heart disease and stroke, the world’s two leading causes of death, are caused by acute tissue ischemia. It is also the cause of decompression sickness, crush injuries, acute compartment syndrome, acute traumatic ischemia, and carbon monoxide poisoning.
Because of the greater oxygen concentrations that are diffused into the tissue following acute exposure to HBOT, blood oxygen levels rise dramatically—by over 1200%, as previously mentioned—allowing more cells in an ischemia-prone location to survive and continue producing ATP. HBOT preserves tissue; it can be used to minimize scarring following elective plastic surgery or to preserve heart muscle during an MI. Only three HBOT protocols over the course of three days were necessary to reduce mortality in users with severe acute traumatic brain injury by 50%, according to a new randomized, placebo-controlled research.
Through the acceleration of all stages of wound healing, HBOT treats wounds anywhere in the body. More than 8,000 genes have their transcriptions altered by it, with genes involved in growth and repair being upregulated and those involved in inflammation and programmed cell death being downregulated. Enhanced leukocyte adhesion, neutrophil function, macrophage killing, and vasoconstricting blood vessels to reduce edema are possible outcomes. Inhibiting apoptotic pathways, repopulating injured areas with newly released bone marrow-derived stem cells, and promoting angiogenesis through VEGF and Hypoxic Inducible Factor (HIF) dependent pathways are means of reducing inflammation.
Large or small, unintentional, age-related, or iatrogenic (from surgery, for example) wounds can all be healed with HBOT. Its capacity to reverse hF and reduce inflammation—which are frequently the primary causes of any wound—is crucial. Consequently, the FDA has authorized HBOT for the therapy of decompression sickness, carbon monoxide poisoning, thermal burns, radiation harm from cancer therapy, and diabetic foot ulcers.
Mitochondrial Impact and Anti-Aging Properties
By giving mitochondria the supraphysiologic levels of oxygen required for cellular respiration, HBOT promotes the production of ATP. HBOT was shown to enhance mitochondrial biogenesis and autophagy in rat hippocampi by partly increasing reactive oxygen species (ROS) generation. New, healthy mitochondria were created throughout this process, whereas outdated, unhealthy mitochondria were eliminated. This rise in antioxidant levels guards against the potentially harmful effects of too many reactive oxygen species.
Antibacterial and Additional Medical Applications
HBOT is a bactericidal antibiotic that works well against facultatively anaerobic and anaerobic organisms. It works best when combined with clindamycin, aminoglycosides, and cephalosporins. It has also been licensed by the FDA to treat chronic refractory osteomyelitis, diabetic foot ulcers (which are frequently superinfected), and necrotizing fasciitis caused by Clostridium Perfringens. It is also an efficient mitigator of endotoxin release in these ailments.
Furthermore, there is evidence that HBOT may be a successful cure for a number of illnesses, including MRSA infections, Lyme disease, small intestine bacterial overgrowth (SIBO), and others.
HBOT Protocols and Duration
Due to the requirement for consistently high oxygen concentrations to induce modifications in DNA regulation and protein transcription, HBOT is usually performed on consecutive days, Monday through Friday, with the weekends off. Depending on the indication, protocols could consist of two therapies or up to 120.
In general, fewer therapies are usually required for the more acute the condition. For plastic surgery users, for instance, three to five sessions are sufficient. The 30- to 60-therapy range is recommended for chronic infections including diabetic foot ulcers, radiation injuries, and post-cranial vasculitis users.